Warwick Davis’s spouse died hours earlier than deliberate hospital discharge, inquest hears | EUROtoday
The spouse of Star Wars and Harry Potter star Warwick Davis died after struggling a cardiac arrest hours earlier than a hospital was planning to discharge her, an inquest has discovered.
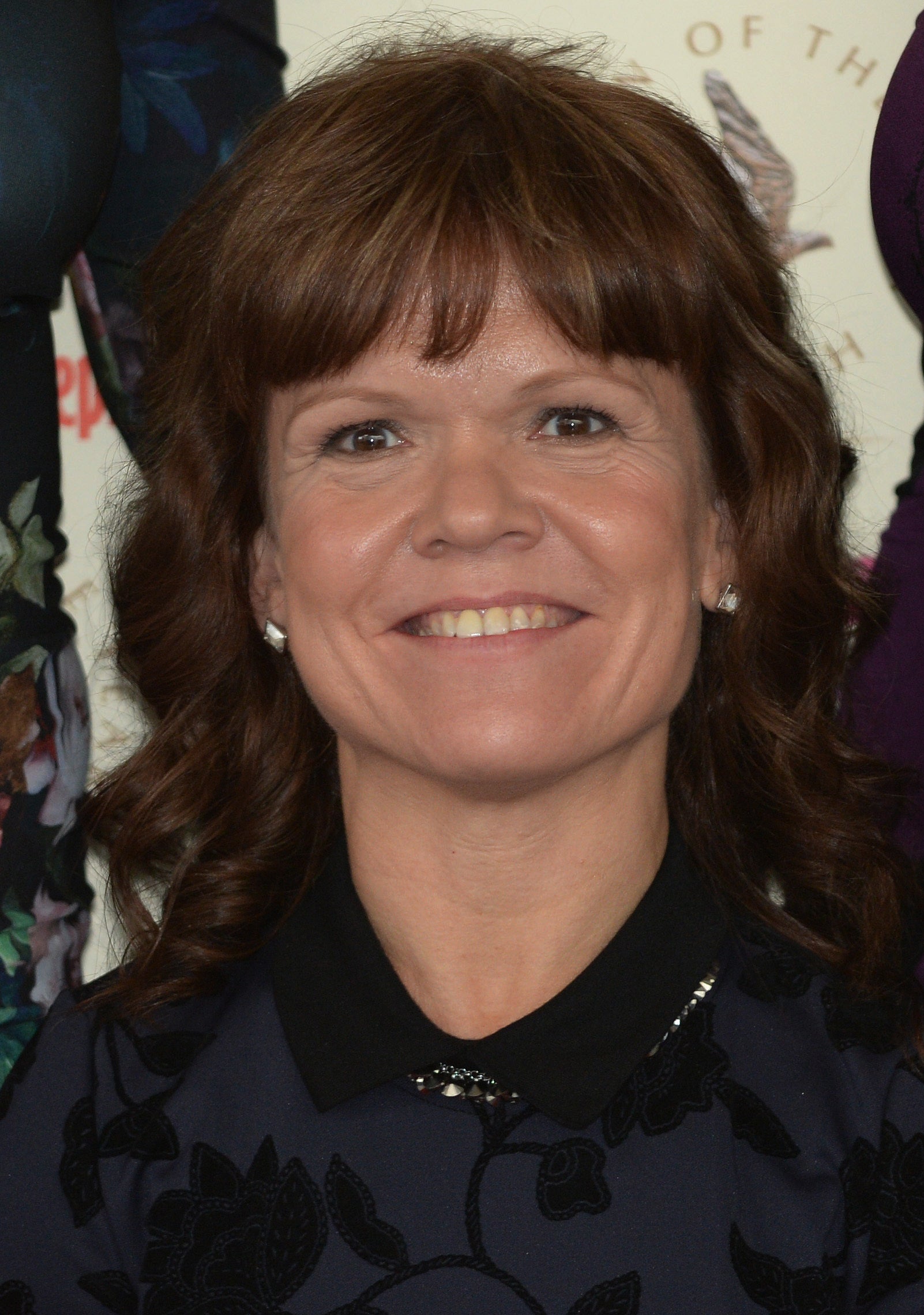
Samantha Davis, who was additionally an actress, died age 53 at University College Hospital in London on March 24 final 12 months, and her inquest was held at Inner West London Coroner’s Court on Monday.
Senior Coroner for Inner West London, Professor Fiona Wilcox, concluded that Ms Davis died of arrhythmic cardiac arrest following problems of important surgical therapy and from achondroplasia “complicated by spinal cord compression”.
Ms Davis was admitted to hospital on February 7 following a sudden lack of mobility in her decrease limbs after a disc prolapse and underwent a thoracotomy operation – a surgical process the place the chest wall is opened – on February 20.
Her situation improved following an additional thoracotomy on March 14 and the University College Hospital at Westmoreland Street was planning to discharge her, the inquest heard.
However, Ms Davis went into cardiac arrest at 11.25pm on March 23 and was pronounced useless at 0.28am on March 24 following a failed try to resuscitate her.
Prof Wilcox stated: “I am satisfied that the medical cause of death should be arrhythmic cardiac arrest and complications following left thoracotomies.
“In my view, the stress of everything together has precipitated this arrhythmic cardiac arrest in a lady who was not known to have any previous arrhythmia problems.”
Prof Wilcox stated Ms Davis had achondroplasia, a bone progress dysfunction which ends up in dwarfism, that was “complicated by very severe spinal problems” requiring a number of surgical procedures from 2016.
Discussing the care she acquired in hospital, Prof Wilcox stated: “I have found nothing but excellent care being delivered to this lady and all of her complications were appropriately managed.
“It is frankly heartbreaking that the surgery itself was successful only for complications to arise and to cause her death.”
David Lawrence, a cardiothoracic surgeon at University College London Hospitals (UCLH), stated Ms Davis’ situation was “progressing well” and he or she had a surgical chest drain eliminated on March 19 and a closing drain eliminated on March 23.
Giving proof, Mr Lawrence stated: “Very sadly, on the night this happened the original plan had been that she would be discharged home the following day.
“We had good evidence that this patient had a chest x-ray that was acceptable, very stable observations and this patient did not bleed during the day.”
Mr Lawrence stated he didn’t imagine the hospital “would have done anything differently”, including that Ms Davis was a “delightful lady”.
Jillian Hartin, lead nurse for affected person emergency response and resuscitation at UCLH, stated employees reported being “out of their comfort zone” in relation to Ms Davis’s cardiac arrest.

Giving proof, she instructed the inquest: “This is a rare event at Westmoreland Street. Since 2020 we’ve only had 14 arrests in five years.”
William Chapman, representing the Davis household, requested Ms Hartin: “Does it surprise you that resuscitation failed given that the team were on the scene quickly?”
Ms Hartin replied: “No, because I think everyone thinks resuscitation works because of television representation of it in dramas.”
Ms Hartin added that the survival fee for non-shockable rhythms was “not good”.
Following a autopsy examination performed on April 5 2024, pathologist Dr John Firth gave Ms Davis’s explanation for demise as being attributable to problems of a left hemothorax, a blood assortment in her lungs, following thoracotomy surgical procedure.
Giving proof to the inquest, Dr Firth stated there was a “significant amount of blood” in Ms Davis’s left pleural cavity across the lungs, including it was unlikely to have been brought on by CPR. Dr Firth stated he noticed no proof that the elimination of the surgical drain brought on a traumatic bleed.
UCLH advisor anesthetist Dr Katharine Hunt instructed the inquest Ms Davis didn’t have a “normal chest” following spinal surgical procedure and thoracotomy. Giving proof, Dr Hunt stated CPR may trigger “extensive damage to tissues within the thoracic cavity”, including that Ms Davis had undergone “very prolonged CPR”.
Mr Chapman stated Ms Davis had phoned her household at 10pm on March 23 and complained of “chest pain”.
He added that the household believed she had suffered a “similar episode” the final time she had a surgical drain eliminated, and likewise raised concern about an “intense physio session” performed hours earlier than her demise.
Mr Chapman stated it was “not ideal” Ms Davis’s therapy was break up between UCLH centres at Westmoreland Street in Marylebone and Queen Square.
https://www.independent.co.uk/news/uk/home-news/warwick-davis-s-wife-died-hospital-discharge-b2733218.html
